This is the fourth in a series of BLG publications to assist Ontario health care providers and organizations to understand and develop governance options as they work toward Ontario Health Team implementation.
OHT Update 4 – September
(PDF, 1.9 MB)
The Connecting Care Act, 2019 (CCA) enables the designation of integrated care delivery systems, which are being referred to as Ontario Health Teams (OHTs). Once designated by the Minister of Health (Minister), the Minister and Ontario Health, the new province-wide agency that is taking on many of the functions of the local health integration networks (LHINs), will treat an OHT like a health service provider for the purposes of the CCA. This means that:
- there can be a single funding and accountability agreement between an OHT and Ontario Health;
- a Minister’s integration order requiring an integration to occur may be issued to or in respect of an OHT; and
- importantly, pursuant to a Minister’s transfer order, an OHT can be the recipient of a transfer of any of the operations of a LHIN, including home care.
OHT participants will include a wide range of different for-profit and not-for-profit entities. The “getting started” model and the “at maturity model” will be self-determined by the team members. The Minister of Health (Ministry) is not prescribing a governance model for OHTs. While it is expected that OHT governance models will evolve over time, at maturity, the Ministry will want a governance model that will provide for a single funding and accountability framework and an organizational framework that can ensure the full continuum of integrated and co-ordinated care for a defined population.
Initially, entities will likely retain their separate autonomy and governance structures, while coming together in a collaborative or shared governance model or decision-making framework to enable achievement of the year one deliverables of the OHT. The year one model is expected to evolve as the work of the OHT expands, however, even at maturity, some OHT members may continue to have separate governance while participating as members of the team. Team member participation at maturity might be through shared governance (such as a joint executive committee), or through contract (such as a service or partnership agreement or funding agreements), or through other arrangements.
What will be important at maturity is to have a “team” structure that:
- is stable;
- operates under a common strategic plan with a central brand; and
- delivers a continuum of integrated and co-ordinated care through a single fiscal and accountability framework with Ontario Health, with a view to achieving the Ministry's "Quadruple Aim".
The Ministry has set out the criteria for OHTs which can be found in the Ministry guidance documentation. The following criteria are particularly relevant when considering the composition of the governance/decision-making framework:
- patients must be involved in the governance model (no guidance on how or what role);
- physicians and clinical leaders are to be involved as part of the OHT’s leadership or governance model; and
- the model must enable the ability to add other providers.
There are key steps to forming an OHT:
- identify team members and their level of participation;
- ensure a shared commitment to the creation of an OHT among team members;
- create a framework for decision-making; and
- document the arrangements.
To assist OHT members in coming together, we have developed the following questions and considerations relevant to the creation of an initial governance model/decision-making framework of an OHT.
Step 1: Identify Participating Providers and Organizations and their Level of Involvement
At the outset, there may be many entities who wish to have a seat at the table. The level of involvement, including the levels of participation in decision-making should be addressed as a principled matter. It likely will not be feasible to design a single decision-making table with all who may want to be team members.
Ask these questions:
- What is the target population at maturity?
- Who are the players in your geographic area?
- What scope of care/support are you interested in coming together to provide in year one?
- Which providers and organizations are critical to that scope of care/support?
- How will primary care be engaged?
- How will patients be involved?
- How will the LHIN be involved?
- What is the role of:
- local partners that have broader mandates (e.g., municipalities)?
- partners that have narrower health-related mandates but larger catchment areas (e.g., province-wide service providers, voluntary sector; specialty facilities; provincial agencies, etc.)?
- How can we keep all potential team members engaged?
Consider various levels of participation such as anchor/lead members, associates/affiliates or supporters/observers, who each may have various means of engagement. Participants may also move between categories over time.
| Team Member | Role |
| Anchor/Lead Member | Year one decision-makers |
| Associate/Affiliate/Engaged | Consulted Have input in decisions May sit on sub-committees May be involved in specific patient/client projects |
| Supporters/Observers/Community | Receive information May attend periodic open forums to receive information and provide input |
Practical Advice
- Initially, the number of participants may be large. Larger teams may impede decision-making and lead to greater challenges in designing a decision-making framework. Studies show that smaller groups (7-12 participants) is optimum for decision-making.
- Principles of inclusion, and considerations of models at maturity may lead groups to be inclusive.
- As specific patient integration initiatives emerge, smaller implementation working groups will form with only those relevant participants engaged.
- The model may need to contemplate various working, strategy and implementation groups to facilitate smaller decision-making forums while continuing to engage all interested participants in larger open sessions.
- Some teams are beginning with fewer participants, particularly where the providers have a history of working together. They will more easily design the initial decision-making framework but it will be important to ensure the team and its structure facilitates expansion through additional participants as the scope of integration activities expands.
Step 2: Confirm Commitment to Participate and Guiding Principles
The Ministry’s initial OHT readiness assessment did not require board approval of the signatory agencies, but did expect confirmation at the highest level of commitment possible. In many cases, the signatory to the readiness assessment was the chief executive officer or executive director. Ensuring that the participating boards are committed and understand the proposed process is a recommended best practice. This can be done through all boards passing a common resolution confirming commitment or it may be evidenced by a non-binding memorandum of understanding (MOU), letter of intent or other similar agreement that is approved by the boards of participating team members.
An MOU ensures that there is a “meeting of the minds” and there is a common agreement on various core elements that will lead to the formation of the OHT governance model/decision-making framework.
The MOU may:
- identify team members;
- if relevant, identify the various participation levels for team members and the implications of such levels;
- confirm the vision to form an OHT that, at maturity, will provide the continuum of integrated and co-ordinated care for a specified geographic area and meet the Ministry’s requirements of an OHT (single clinical and fiscal accountability framework);
- confirm the team members’ intention to:
- work collaboratively to complete the full application process; or
- if identified by the Ministry as “In Discovery” or “In Development”, work collaboratively towards being asked to complete the full application process; or
- if no readiness assessment was submitted, work collaboratively with a view to submitting a future readiness assessment.
- set out any agreed core requirements and the process to achieve the Ministry’s requirements for an OHT;
- establish a working group for the purposes of completing the work for the full application or readiness assessment. This group may be charged with recommending a “getting started” governance model/decision-making framework. The model and framework may be set out in the MOU or left to the working group to determine. The parties may have decided to retain a facilitator or neutral chair and that may be set out in the MOU or left to be a decision of the working group;
- commit to an initial set of guiding principles, which might include:
- patient/client focus;
- system approach (system ahead of organizations);
- inclusivity;
- equal voices;
- consensus decision-making. (Note: There may be different decision-making principles once the structure is formalized);
- trust; and
- transparency.
- agree to make joint approaches to third parties; and
- agree on any cost sharing.
Practical Advice
- Some groups may have moved beyond the stage of benefiting from an MOU, particularly if they have a history of working together and have formed a strong working group to submit a readiness assessment. In these cases, the group may be moving to formalize a decision-making structure as discussed at Step 3 below.
- For groups that are farther away from being asked to submit a full application, the MOU may enable the identification of collaboration opportunities to provide more integrated care, and such integrations of care may be specific projects subject to their own definitive agreements involving subsets of the participants.
Additional Considerations: Coming Together and Building Trust
- Is there a history of successfully working together?
- Is there trust? Do steps need to be taken to build trust?
- Can the team members do this on their own, or do the parties need to work with a facilitator to find a preferred model?
- Are the team members coming together as equals?
- What stakeholder engagement processes will be needed? Consider: patients, donors, volunteers, employees, local government, clients, other health services providers, etc.
- How will the structure allow for the addition of new team members?
Step 3: Develop a Governance Model or Decision-Making Framework
The Ministry has asked applicants to describe their year one governance structure and whether it is transitional. If the team has not yet decided upon the structure, then it must inform the Ministry of its plan to formalize the working relationships among the team members, including:
- shared decision-making;
- conflict resolution;
- performance management;
- information management;
- information sharing;
- resource allocation; and
- the extent to which new members can be accommodated.
The Ministry has indicated that current funding arrangements will stay in place and we assume that OHT participants will likely maintain their separate legal entities while coming together over a shared vision. It is possible that some entities with similar missions may voluntarily decide to integrate more formally but there is no requirement or expectation for that to occur at this stage.
There are a number of options available for the year one model, including:
- committee or working group arrangement;
- governing group established under a collaboration or joint venture agreement;
- joint executive committee; or
- single governance corporation supported by a membership agreement.
There are a number of considerations for designing the decision-making framework:
- Composition:
- Size of group?
- Comprised only of representatives from Anchor/Lead team members? Management or board or both?
- Will any neutral ‘outsiders’ be included?
- Who selects?
- Are designates/substitutes permitted?
- How are patients/clients involved?
- How are physicians involved?
- Chair:
- A neutral(outside) chair?
- Rotating chair (annually or by meeting) or best person for the role?
- Co-chairs?
- Members pick from among themselves?
- Decision scope:
- Advisory or decision-making body or both depending on issue?
- What requires a decision of the team member boards?
- How are sub-committees established?
- Decision-making process:
- Defined consensus, or majority or supermajority?
- Process to break a tie?
- Quorum?
- Meeting frequency? In person or electronic?
- Dispute resolution:
- Principles to avoid disputes from developing?
- Process to resolve, including exchange of issue statements, role of CEOs and board chairs?
- Mediation with neutral facilitator?
- Does process vary depending on nature of dispute?
- Form to follow function and evolve:
- Periodic review?
- Concept of governance in timeframes: 0-12 mo; 12-24 mo; 3-5 yrs?
Practical Advice
- Whether a decision is made to create a governing corporation with a board of directors, to move forward with a less formal steering or collaboration committee, or something in between such as a joint venture management board or joint executive committee with decision making authority, there will be a group of individuals who are representative of the Anchor/Lead team members who come together to make decisions.
- In some cases, the decisions may be within a scope that the team members have agreed can be made by that decision-making body and move to implementation, or they may take the form of recommendations back to the boards of the team members, or both. Different team member boards may have different levels of delegation to management. Where one team member board may require approval, another may not.
- A determination will need to be made as to the role of the members of the boards of the team members. Are they receiving and reacting to reports from the governing body of the OHT or are they sitting as members of the OHT governing body? There may be a role for members of boards on a governance sub-committee or communication and engagement sub-committee. Given the nature of the year one work, we expect most OHTs will start with a decision-making group that is management-led.
- Some models might involve a two-tiered structure with a governing body of the OHT comprised of board and management from team members with an executive management committee comprised of CEOs/CFOs/executive directors or their designates. The executive management committee would operate as an operational committee while the OHT governing committee would operate in a steering and oversight role. This structure provides for more board engagement but may not be as nimble in year one.
- In addition, there will be a number of “working groups” or “task forces” that will need to be identified. Examples of these might include innovation, digital, governance, communication and engagement. They will provide an opportunity for involvement of participants within the geographic region who are not Anchor/Lead members. One option for board-level engagement might be a "Chairs Council" comprised of board chairs and vice-chairs.
- Another important practical consideration is the documentation around implementation of specific patient care integrations. As the OHT decision-making framework identifies opportunities to integrate patient/client care, those team members involved in such opportunities may sign a “statement of work” or other implementation agreement to document specific arrangements. Only those team members involved in that particular integration would need to be signatories to that documentation; however, reporting and oversight would be the role of the OHT governing/decision-making body.
Additional Considerations: Communication and Engagement
Adopting a communication strategy early in the process is critical to keep key stakeholders informed and engaged. Some providers and organizations may adopt a process that allows questions to be submitted and answers published as a way of managing information and dispelling false or misleading information. The communication strategy needs to consider both internal and external stakeholders. Key questions to ask include:
- To whom should we communicate and for what purposes?
- What detail is required?
- How often should regular update messages be provided?
- How can we manage false or misleading information?
Step 4: Memorialize the Governance Model for OHT Development
Options for documenting the governance/decision-making framework for the OHT will include:
- Terms of Reference for a joint steering/collaboration committee and, if established, a joint executive management committee;
- Collaboration Agreement or Joint Venture Agreement or Governance Agreement;
- Joint Executive Committee Agreement with Terms of Reference for a Joint Executive Committee;
- Members' Agreement and by-laws (if a corporation is formed).
Considerations in determining which form of documentation is most suitable will depend in part on the degree to which the arrangements are formal or informal and binding or non-binding.
Documentation may be limited to what is required to reach decisions with implementation dealt with in separate agreements or statements of work with only team members involved in that project as a party.
Additional Considerations: Implementing Patient Centred Integrated Care and Resources and Risks
- How will other working groups be established and what will be the reporting relationships?
- How will specific patient/client initiatives be implemented? What documentation and support will be required?
- How will the governance arrangement be supported?
- What is being considered in respect of sharing or secondment of employees?
- Are there any labour and employment implications?
- Are there new risks/liabilities? Is there a need for a legal structure as a risk mitigation strategy?
- Are all team members charities? Is tax advice required if assets are shared or payments or transfers made between parties? HST considerations?
- What do the team members need to know about one another before proceeding? What due diligence is prudent?
- Is stability an objective? Should there be a minimum term or an indefinite term with opportunity to re-visit at a fixed date (two years, five years, ten years)? Is the objective a term-limited structure or “an egg that cannot be unscrambled”?
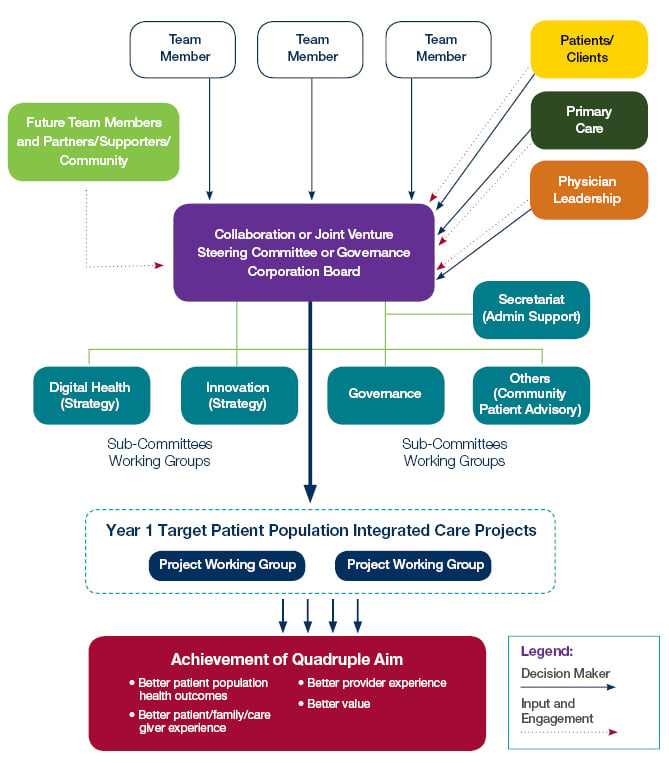
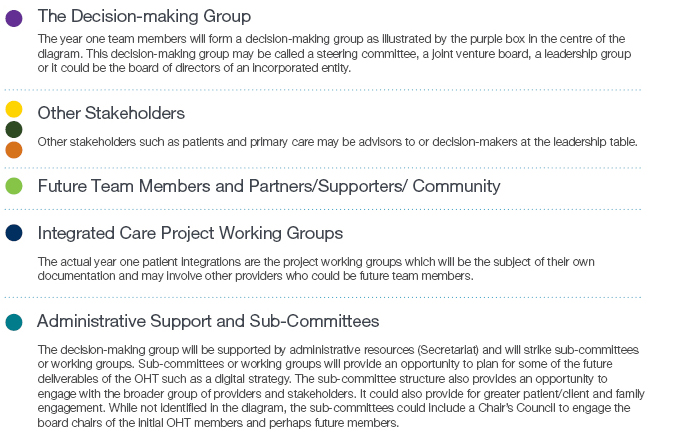
OHT Potential Year One Governance Model
The following diagram provides a “Year One” governance/decision-making model that will allow for various levels of participation and enable implementation of integration for the year one targeted patient population. A description of this diagram follows below.
Additonal Resources
BLG has released:
- Governance Options: Getting Started and Evolving Towards Maturity (April 2019), which describes options for OHT governance;
- Governance Best Practices for High Performing Health Provider Boards (August 2019), which describes governance best practices relevant to OHT participants; and
- Forming Ontario Health Teams: The Role of the Health Provider Board (August 2019), which provides guidance on core elements of an OHT governance framework in year one.


